Alcohol Use Disorder (AUD)
What is Alcohol Use Disorder?
Alcohol use disorder (AUD), a substance use disorder (SUD), is a medical condition defined by the DSM-5 as “a problematic pattern of alcohol use leading to clinically significant impairment or distress,” and is diagnosed as either mild, moderate or severe depending on the number of symptoms (out of a possible 11) that are present within the past 12 months (NIAAA, 2024). The World Health Organization (2024) estimates that 400 million people (or 7% of the world’s population) suffer from Alcohol Use Disorder.
It is important to note that referring to the condition as alcohol abuse or alcoholism may increase stigma, which then can exacerbate AUD (NIAAA, 2024). Shame, identity issues, and a lack of knowledge about treatment underlie this stigma. This, in turn, negatively impacts the individual’s emotional state, which drives the AUD, and deters them from seeking treatment.
Related Tags for Resources:
Alcohol, Alcohol Use Disorder, Al-Anon, Alcoholics Anonymous, Drinking Culture, Medication-Assisted Treatment, Recovery, Relapse
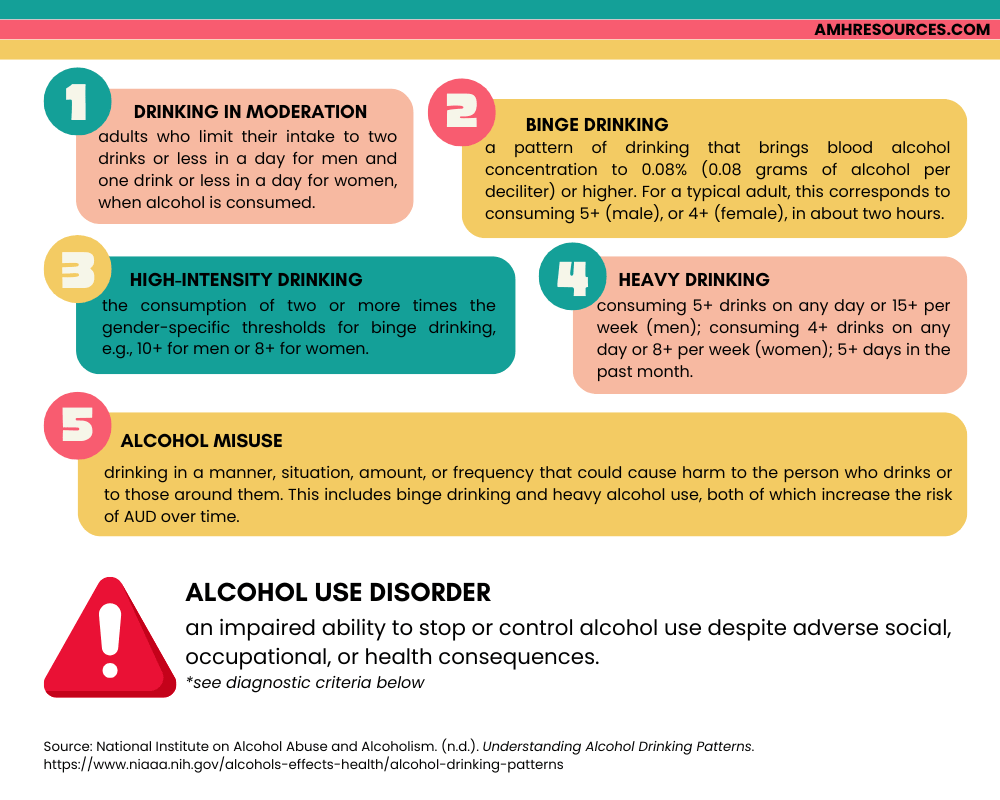
Understanding Alcohol Consumption Levels
Drinking Patterns
Unfortunately, many people are unfamiliar with the concept of a standard drink and even those who are aware still find it difficult to calculate. In fact, a 2023 survey showed that 70% of participants were not able to correctly identify how many standard drinks were in various alcoholic drinks. This problem, coupled with scientific evidence that shows that any amount of alcohol can present health risks, makes it crucially important for the average consumer to educate themselves, and for the government (e.g., policies) and companies (e.g., packaging) to play an active role as well.
What Is a Standard Drink?
This is important because the liver can only process so much alcohol - the remaining can cause harm to the liver and other organs as it moves throughout the body. Additionally, those serving alcohol need to be aware of how much each customer has consumed. Lastly, using standard drink sizes to measure alcohol consumption can help the individual and professionals in their discussions of alcohol misuse / alcohol use disorder.
I recommended searching up the standard drink sizes for your country if it is not on this short list. If you need any help, feel free to contact me.
Australia, Canada, Ireland, United Kingdom, United States
2. Drinking Guidelines: General Population
3. Knowing Your Limits with Alcohol: A Practical Guide to Assessing Your Drinking [PDF]
4. Light to Moderate Intake of Alcohol, Drinking Patterns, and Risk of Cancer
5. Patterns of Alcohol Abuse
6. What is a Standard Drink?
Diagnosing AUD
- Withdrawal, as manifested by either of the following:
- (A) The characteristic withdrawal syndrome for alcohol
- (B) Alcohol (or a closely related substance, such as a benzodiazepine) is taken to relieve or avoid withdrawal symptoms.
- Alcohol is often taken in larger amounts or over a longer period than was intended.
- There is a persistent desire or unsuccessful efforts to cut down or control alcohol use.
- A great deal of time is spent in activities necessary to obtain alcohol, use alcohol, or recover from its effects.
- Craving, or a strong desire or urge to use alcohol.
- Recurrent alcohol use resulting in a failure to fulfill major role obligations at work, school, or home.
- Continued alcohol use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of alcohol.
- Important social, occupational, or recreational activities are given up or reduced because of alcohol use.
- Recurrent alcohol use in situations in which it is physically hazardous.
- Alcohol use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by alcohol.
- Tolerance, as defined by either of the following:
- (A) A need for markedly increased amounts of alcohol to achieve intoxication or desired effect
- (B) A markedly diminished effect with continued use of the same amount of alcohol.
Specify whether the client is:
- In early remission: after the full criteria for AUD were previously met, none of the criteria for AUD have been met for at least three months but for less than 12 months
- In sustained remission: after the full criteria for AUD were previously met, none of the criteria for AUD have been met at any time during a period of 12 months or longer
- In a controlled environment: if the individual is in an environment where access to alcohol is restricted.
Specify current severity:
- Mild: presence of 2-3 symptoms
- Moderate: presence of 4-5 symptoms
- Severe: presence of 6 or more symptoms
References: NIAAA (2024) & RAND (2021)
Statistics
• 2 million of these deaths were men.
• 13% of these deaths affected younger people aged 20 to 39 years old.
• The proportion of people with AUDs in contact with treatment services is low - ranging from 1% to 14% depending on the country.
• 1 in 10 children live with a parent with AUD.
• AUD is 3-4x higher in families where a relative has AUD.
• About 3% of youth ages 12 to 17 had AUD in the past year.
• It is the 4th leading cause of preventable death in the U.S.
• Less than 5% of Americans with a diagnosis receive any treatment.
References: American Psychiatric Association (n.d.) & World Health Organization (2024)
2. Alcohol Consumption Statistics (EU)
3. Alcohol Use Patterns Among Urban and Rural Residents
4. Alcohol use and burden for 195 countries and territories, 1990–2016
5. Canadian Alcohol and Drugs Survey (CADS)
6. Canada’s Guidance on Alcohol and Health [PDF]
7. Global burden of 87 risk factors in 204 countries and territories, 1990-2019
8. Global status report on alcohol and health
9. National Institute on Alcohol Abuse & Alcoholism - Facts & Statistics (U.S.)
10. The epidemiology of alcohol use disorders cross-nationally: Findings from the World Mental Health Surveys
Causes & Risk Factors
Psychological
Certain psychological conditions can increase the likelihood that someone will develop an AUD (Addiction Center, 2024). For example, those with depression, social anxiety, and bipolar disorder are more likely to develop AUD. Psychiatric disorders that present deficits in executive function (e.g., attention-deficit/hyperactivity disorder) or negative affect (e.g., depression, anxiety) are at an increased risk for developing AUD (NIAAA, 2024). More specifically, AUD is prevalent in 20-40% of those being treated for an anxiety disorder and up to 40% for major depressive disorder. About 15-30% of people with AUD also have post-traumatic stress disorder; 40-50% have had another substance use disorder; and up to 91% have a sleep disorder.
Many individuals with a psychological illness(es) turn to alcohol and/or other substances as a way to cope with their disorder (Addiction Center, 2024; NIAAA, 2024). A history of trauma, regardless of the type of trauma, presents an increased risk for abusing alcohol (Brady & Back, 2012). Furthermore, the disorders themselves impair someone’s ability to recognize the reality of their drinking and to acknowledge the risks and warning signs associated with their drinking (NIAAA, 2024).
2. Alcoholism and Psychiatric Disorders
3. Co-Occurring Alcohol Use Disorder and Schizophrenia
4. Mental Health Disorders And Alcoholism: Dual Diagnosis
5. Mental Health Issues: Alcohol Use Disorder and Common Co-occurring Conditions
6. Self-Medicating Anxiety with Alcohol: What You Need to Know
7. The Relationship Between Alcohol and Depression with Psychiatrist Dr. Paul Linde
8. The Role of Stress in Alcohol Use, Alcoholism Treatment, and Relapse
9. The Truth About Severe Anxiety And Alcohol Abuse
10. What is the link between alcohol use disorder and mental health conditions?
11. What is the relationship between anxiety and alcohol use?
Age
Alcohol use tends to begin in late adolescence and early twenties, peaks in middle to late twenties, and begins to slow by early thirties (Addiction Center, 2024). Those in their early to mid-twenties are the most likely to develop an AUD. Furthermore, the younger a person is when they begin to drink, the more likely they are to develop AUD later in life – this is especially true if they start before the age of 15.
Heavy drinking during adolescence can negatively impact critical brain development (see: NIAAA). It is also associated with other risky behaviours, such as drug use, unprotected sex, academic problems, impaired driving, conduct problems, suicide, and increases the likelihood of developing an AUD in adulthood. Furthermore, research suggests that rates of anxiety and depression are increasing among adolescents, especially girls, who are more likely to use alcohol to cope with these conditions (White, 2020). Research also shows that alcohol use and alcohol-related harms are increasing among older people (ages 55 to 75), with increases being larger for women.
2. Alcohol Use in the United States: Age Groups and Demographic Characteristics
3. Differences in alcohol use between younger and older people: Results from a general population study
4. Drinking patterns and risk behaviors associated with combined alcohol and energy drink consumption in college drinkers
5. Facts About Aging & Alcohol Use
6. Underage Drinking, Dangers and Consequences
7. Under Construction: Alcohol and the Teenage Brain
Family & Genetic
The genetic implications of AUD have been widely studied. In addition to influencing AUD, genetic factors also contribute to alcohol consumption levels, alcohol metabolism, hangover severity, alcohol-associated diseases and more (Edenberg & Foroud, 2013; Addiction Center, 2024).
There is no singular gene that leads to the development of AUD as many genes and variations of genes have been shown to impact risk (American Addiction Centers, 2024). In fact, research has discovered at least 51 genes that impact AUD (Addiction Center, 2024).
Although up to 50% of the reason why someone develops an AUD can be attributed to a family history of the disorder, it is not a guarantee (Addiction Center, 2024). Epigenetics, which is the interaction of genes and the environment, and social factors play a significant role in AUD as well.
2. The Effect of Genetic Variation on Outcomes for Alcohol Dependence Treatment
3. Traits That Come From Growing Up With Alcoholic Parents
4. Vulnerability Factors For Alcoholism [PDF]
5. Wasted: Exposing the Family Effect of Addiction
Sex & Gender
Sex and gender are distinct constructs – sex refers to biological factors whereas gender refers to social and cultural factors (Gilbert et al., 2018). Research has shown that biological factors (e.g., hormones, fat and muscle composition, and body water content) differ by sex, and these differences affect alcohol metabolism and the risk of a variety of negative consequences. Additionally, physiological sex characteristics can shift for many transgender individuals who undergo gender-affirming treatments, such as hormone therapy. This, however, is still a new area of research.
Gender, on the other hand, is a social construct that involves many characteristics, such as feelings, behaviours, preferences, perceptions, and social relationships (Gilbert et al., 2018). Gender influences drinking behaviours, such as the onset of drinking, the frequency and quantity of drinking, and the risk of AUD. Research has found that several alcohol-related behaviours are more likely to be predicted by certain gender-related characteristics (e.g., personality traits and social roles) than physiological sex characteristics.
Globally, men consume more alcohol than women and have more alcohol-related harms to themselves and others (White, 2020). However, there are large variations in gender gaps in alcohol use between countries, suggesting that culturally prescribed gender roles significantly shape gender-specific drinking patterns. Lower levels of alcohol consumption harm women at higher rates than men (NIAAA, 2024). For example, even with fewer years of AUD, women perform more poorly than men on a variety of cognitive tasks. They are also at a greater risk for many alcohol-related health problems, such as cardiovascular disease, liver inflammation, and certain cancers.
2. Gender Differences in Moderate Drinking Effects
3. Gender Differences in the Psychosocial Determinants Underlying the Onset and Maintenance of Alcohol Use Disorder
4. Sex Differences in Alcohol Consumption and Alcohol-Associated Liver Disease
5. Why alcohol affects women more than men
6. Why Biology Matters When it Comes to Drinking Alcohol [PDF]
LGBTQ+
Studies have found that the risk for developing AUD is far greater in women who are sexual minorities (based on their sexual identity, behaviour, or attraction) than in heterosexual women (NIAAA, 2024). For example, lesbian and bisexual women are twice as likely as their heterosexual counterparts to engage in binge drinking (White, 2020). The likelihood of AUD is similar for homosexual and heterosexual men (NIAAA, 2024).
Alcohol misuse is highly prevalent in transgender populations, with a 2015 survey indicating high rates of binge drinking in general, but much higher levels in transgender communities of colour (Gilbert et al., 2018). However, it is important to note that their gender identity is not the source of risk, but rather, the societal discrimination and stigma that they face creates psychosocial conditions that heavily increase the risk of problematic alcohol use (Hatzenbuehler et al., 2013). Furthermore, these individuals also experience more secondary harms, such as being victims of violence, ranging from sexual and physical assault to verbal abuse (Gilbert et al, 2018).
2. Alcohol & Queerness
3. Alcohol Addiction & Substance Abuse in the LGBTQ Community
4. Alcohol Research With Transgender Populations
5.Drug and Alcohol Addiction in the LGBT+ Community
6. LGBTQ Alcoholism
7. LGBTQ+ People & Alcoholism [PDF]
8. Out in the Open: Alcohol Use & Harm in LGBTQ+ Communities [PDF]
9. Problematic Alcohol Use Among Gay, Bisexual, and Other Men Who Have Sex With Men in Canada: The Role of Proximal Stressors and Anxiety
10. The Influence of Gender and Sexual Orientation on Alcohol Use and Alcohol-Related Problems
Education & Career
Alcohol consumption is more likely in those who are more highly educated (Addiction Center, 2024). In the U.S. for example, 80% of college graduates drink, whereas 52% of non-college students drink. Certain professions are more likely to develop AUD, especially those in high-stress and/or high-risk careers (e.g., military members).
2. Binge Drinking and Academic Performance
3. Educational Attainment Impacts Drinking Behaviors and Risk for Alcohol Dependence
4. Educational Level and Alcohol Use in Adolescence and Early Adulthood
5. Is It Workplace Stress a Trigger for Alcohol and Drug Abuse?
6. The Workplace and Alcohol Problem Prevention
7. Work Stress and Alcohol Use
Religion
Although anyone of any religion can develop AUD, those who adhere to strict religious values that strongly oppose alcohol use are less likely to drink and therefore develop AUD (Addiction Center, 2024). This is particularly true when the religion plays a significant role in influencing the availability of alcohol, social practices, and local laws.
2. Religion & Drinking
3. Religiosity, Race/Ethnicity, and Alcohol Use Behaviors in the United States
4. Religious Beliefs & Alcohol Control Policies: A Brazilian Nationwide Study
5. Religious Factors Associated with Alcohol Involvement
6. The Evolution of Wine in Christian vs. Islamic Theology
7. What Does the Bible Say About Alcohol?
8. What Different Religions Say About Alcohol
9. What’s the Difference Between Christian Denominations on Alcohol?
10. Why Is Alcohol Prohibited in Hinduism?
11. Wine Consumption & Religions
Social & Cultural
North American culture is one that celebrates alcohol use – it is considered ‘normal’ for teenagers to experiment with alcohol, is a ‘rite of passage’ when becoming an adult, is normalized at family functions, such as birthdays and holidays, and is a significant component of post-education. For example, “hazing” is a long-standing tradition in fraternities, often involving high levels of alcohol use (Ing et al., 2024). Russia has the highest level of alcohol consumption in the world – drinking is a pervasive and socially acceptable behaviour, and despite the widespread problems it has caused, alcohol is a major source of revenue for the government (Korotayev, 2008). Women in more developed countries drink more than women in developing countries (Rehm et al., 2009). (See also: Wikipedia – Drinking Culture).
An individual’s drinking habits are strongly influenced by the environments in which they live and work (Addiction Center, 2024). Research has documented the relationship between social determinants of health (SDH) and alcohol use (Sudhinaraset et al., 2016). Living in an unhealthy environment, whether mentally or physically, presents an increased risk. It is important to be aware of how the various SDHs can influence an individual’s likelihood of developing any substance use disorder (Swan et al., 2021). These include having family members and/or peer networks that engage in alcohol abuse, living and/or working in unsafe conditions, a lack of housing and/or financial security, lower socioeconomic status, a history of abuse and/or trauma, a lack of positive social supports, and prior health conditions.
Socioeconomic status indicators (SES; e.g., income, occupation, education) are strong predictors of health behaviours, such as alcohol use (Sudhinaraset et al., 2016). A higher SES is associated with more frequent drinking, but lower SES is associated with larger amounts of alcohol. Social Capital Theory suggests that health is highly influenced by the quality of one’s social networks and connections, with higher levels of social support and community cohesion resulting in better health outcomes.
Bronfenbrenner’s Ecological Systems Theory is useful in explaining these influences on AUD. Each of these levels present a variety of risk and protective factors in the development of AUD (Sudhinaraset et al., 2016). At the individual level, there are personal factors such as SES and race/ethnicity. At the microsystem level, you have the family and home environment (e.g., parental alcohol use) and peer networks, which are situated in the larger community (e.g., societal norms). This, then, is embedded into the macro-level, where exposure to alcohol through advertisements, as well as laws and policies, influence alcohol use. Media exposure (e.g., television, movies, social media and so on), for example, has been linked to alcohol consumption levels and it is likely that the effects of this differ across socio-cultural groups.
Discrimination & Stigma
On a final, but very important note, discrimination and stigma has been linked to risky health-related behaviours (Sudhinaraset et al., 2016). As an uncontrolled and unpredictable source of stress, discrimination is incredibly harmful to health (Pascoe & Richman, 2009). The psychological implications of experiencing discrimination and stigma lends itself to a stress and coping framework – in other words, the experience of discrimination and stigma results in psychological problems (e.g., depression, anxiety, and so on) that leads to stress and individuals then must find a way to cope with that stress. This is one reason why many people abuse alcohol.
2.Alcoholism: The Deadly Truth About Its Stigma
3. Associations Between Socioeconomic Factors and Alcohol Outcomes
4. Embodying Inequality: A Review of Concepts, Measures, & Methods for Studying Health Consequences of Discrimination [PDF]
5. Socioeconomic Position Indicators and Risk of Alcohol-Related Medical Conditions
Treatment, Recovery & Relapse
Detox & Withdrawal
The first step in treatment AUD is for the individual to safely detox and withdrawal from alcohol (Addiction Center, 2024). Alcohol withdrawal is incredibly dangerous because of the effect it has on the brain and body. More specifically, withdrawal symptoms are the opposite of the symptoms experienced when drinking – for example, as a depressant, alcohol causes bodily processes to slow down, but when someone is in withdrawal, the symptoms are stimulating and sped up (thus the “shakes”).
Withdrawal from substances is typically not life-threatening, but alcohol is the exception. The following symptoms are not exhaustive. Within 6 to 12 hours, the patient begins to tremors, nightmares, and insomnia; 12-24 hours hallucinations and intense fear; 24-48 hours presents a high risk for seizures; 48-72 delirium, fever, irritability, confusion; and 72-96 hours presents the highest risk for delirium tremens.
Behavioural Treatments
These are aimed at changing behaviour through counselling. One prominent kind is Cognitive-Behavioural Therapy, which helps clients recognize and work through the distorted thoughts patterns that influence their behaviours and thus their AUD (Anderson, 2023). Another one is Dialectical Behavior Therapy (DBT). This article by Flanagan et al. (2018) provides a fantastic overview into various treatments.
Medications
These are used during all stages of treatment, from detox to sobriety. The most well-known medication is Naltrexone, which must be given after detox. This medication binds to endorphin receptors and therefore blocks the effects of alcohol – reducing cravings and the amount of alcohol consumed. This treatment lasts for about 3-4 months. There is also Acamprosate, which reduces post-acute withdrawal symptoms, and Disulfiram, which causes unpleasant symptoms (e.g., nausea) when someone consumes alcohol. For a more exhaustive list, view this article.
Mutual Support Groups
Alcoholics Anonymous is a peer-led, global fellowship dedicated to abstinence-based recovery (Wikipedia). It uses a spiritually-inclined twelve-step program wherein self-improvement and recovery is beleived to occur by following the will of a self-defined “God as we understood Him .” The first step is to admit you are powerlessness over alcohol and recognize the unmanageability of your life due to your drinking. There are two other subsets of this program: Al-Anon is for the family and friends of the alcoholic and Alateen is specifically for teenagers who have been affected by someone’s drinking.
Relapse Prevention
This is an essential aspect of the recovery process from any addiction. Relapse is a process rather than a singular event (Guenzel & McChargue, 2023). There could be an emotional relapse, a mental relapse, or a physical relapse, all of which can occur during any stage of recovery (for more information on the stages of change, view this article).
Melemis (2015) wrote an article on relapse prevention and the five rules of recovery that I believe is very important to read in order to understand relapse / prevention. These rules are: change your life (recovery involves creating a new life where it is easier to not use); be completely honest; ask for help; practice self-care; and don’t bend the rules.
Lastly, many view a lapse and relapse differently: A lapse is often seen as a normal part of recovery, where an individual uses again but recovers within a short time frame. A relapse is a resurgence of full-blown addictive behaviors, suggesting the need to take inventory, reassess, and re-engage with treatment (CAMH, n.d.; Washburn House, 2021).